In-Depth Exploration of Bilateral Salpingo-Oophorectomy: A Vital Procedure in Women's Healthcare
In the realm of women's health, surgical procedures that address complex gynecological issues are crucial for preserving and enhancing well-being. Among these, bilateral salpingo-oophorectomy stands out as a significant operation with a profound impact on a woman's health trajectory. Leading obstetricians and gynecologists at drseckin.com are dedicated to providing comprehensive care, expert advice, and innovative surgical solutions for women facing gynecological health challenges.
Understanding Bilateral Salpingo-Oophorectomy: Definition and Overview
Bilateral salpingo-oophorectomy is a surgical procedure that involves the removal of both fallopian tubes (salpingectomy) and ovaries (oophorectomy). This operation is typically performed to treat or prevent various gynecological conditions, including ovarian cancer, benign cysts, endometriosis, or as a prophylactic measure in women with significant genetic risk factors.
The procedure is a strategic intervention designed to eliminate sources of ovarian or fallopian tube pathology, significantly reducing the risk of certain cancers and alleviating symptoms associated with gynecological disorders.
The Medical Indications for Bilateral Salpingo-Oophorectomy
This surgery becomes necessary under specific clinical circumstances, including:
- Ovarian or fallopian tube cancer: To remove malignant tissues and prevent spread.
- High genetic risk: Women with BRCA1 or BRCA2 mutations often opt for this preventive surgery to drastically lower their cancer risk.
- Persistent ovarian cysts: Particularly cysts that do not resolve with conservative management.
- Severe endometriosis: When the disease significantly affects ovarian function and quality of life.
- Chronic pelvic pain: When attributed to ovarian or tubal pathology unresponsive to other treatments.
- Pelvic infections or adhesions: That compromise adnexal health and function.
The Surgical Procedure: Step-by-Step Process
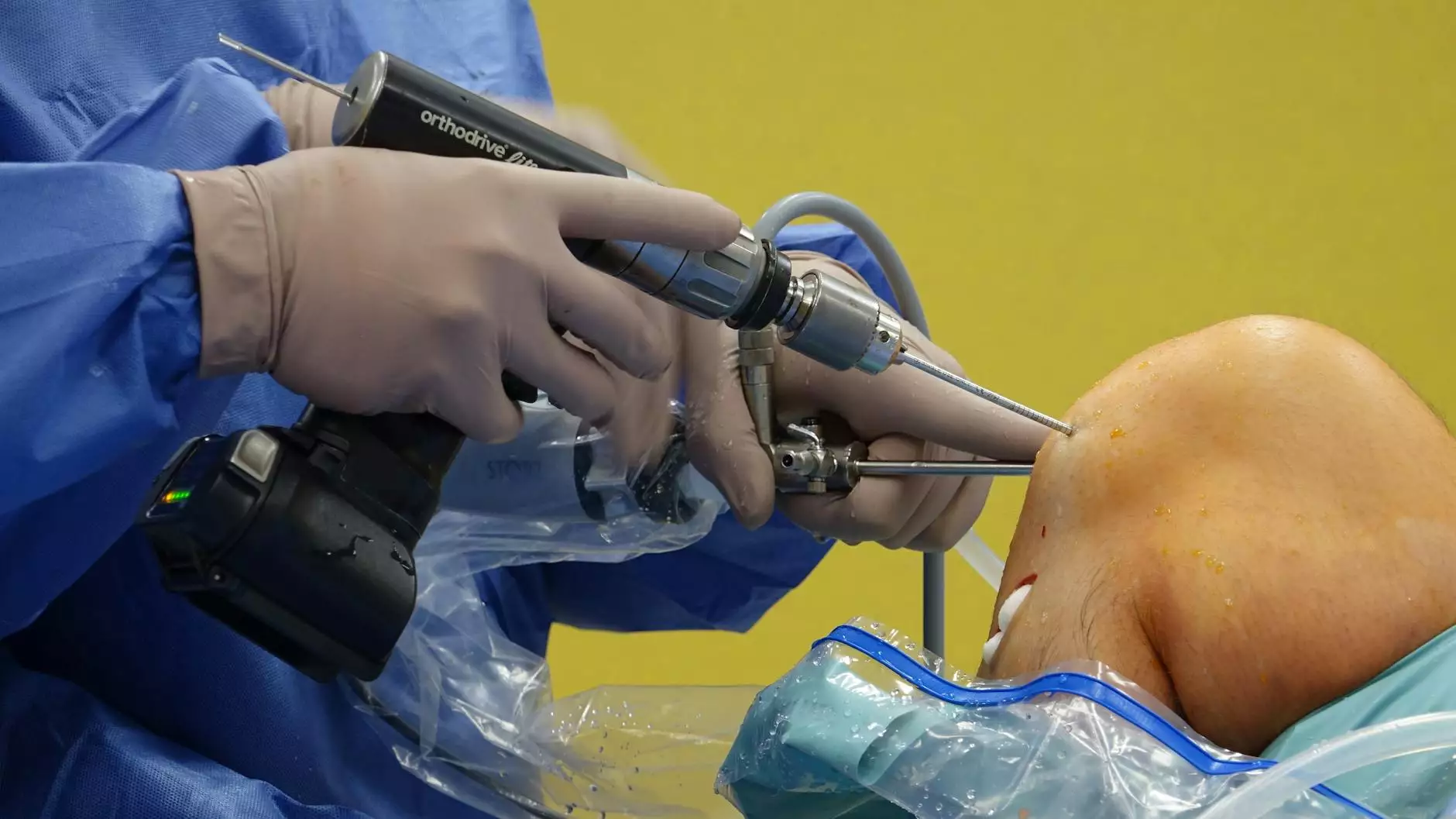
The bilateral salpingo-oophorectomy procedure can be performed via various approaches, including laparotomy (open surgery), laparoscopy (minimally invasive), or robot-assisted surgery, each tailored to the patient's specific condition.
Preparation and Preoperative Evaluation
Prior to surgery, comprehensive assessments are conducted, including pelvic ultrasound, blood tests, and genetic screening if indicated. Women are advised to discuss medication use, allergies, and medical history thoroughly with their surgeon.
The Surgical Technique
In most cases, the surgeon creates small incisions in the abdomen. Using a laparoscope— a thin, lighted tube— the surgeon visualizes the pelvic organs. The fallopian tubes and ovaries are carefully dissected from surrounding tissues, ensuring minimal trauma and bleeding. The excised tissues are then removed through the incisions or a specialized retrieval bag.
The entire procedure is performed under sterile conditions and general anesthesia, with the goal of reducing recovery time and post-operative discomfort.
Postoperative Care and Recovery
Following the surgery, women typically stay in the hospital for a few hours to overnight, depending on the surgical approach and individual health status. Recovery involves managing pain, monitoring for signs of infection, and gradually resuming normal activities. Patients are advised to follow their surgeon’s guidelines carefully to ensure optimal healing.
It's important to recognize that bilateral salpingo-oophorectomy induces menopause if performed before natural menopause age. Women should discuss potential hormonal effects and management strategies with their healthcare provider.
Risks and Benefits of Bilateral Salpingo-Oophorectomy
Advantages
- Significant reduction in ovarian and fallopian tube cancer risk, particularly for high-risk women.
- Symptom relief from ovarian cysts, endometriosis, or chronic pelvic pain.
- Prevention of recurrence of certain benign or malignant conditions.
- Potential for early detection and intervention in women with familial cancer syndromes.
Potential Risks and Considerations
- Hormonal changes leading to menopause symptoms such as hot flashes, night sweats, and mood swings.
- Bone density loss increasing osteoporosis risk if hormone levels decline.
- Cardiovascular risk which necessitates lifestyle adjustments and medical management.
- Infection, bleeding, or injury— typical surgical risks.
- Impact on fertility— this is a definitive loss of reproductive capacity.
Long-Term Considerations and Hormonal Management
For women who undergo bilateral salpingo-oophorectomy at a premenopausal stage, hormonal replacement therapy (HRT) is often recommended to mitigate menopausal symptoms and protect bone health. The decision regarding HRT should be personalized, considering the patient's overall health, risk factors, and preferences.
Close follow-up with women’s health specialists ensures optimal management of long-term health consequences, including cardiovascular health, bone density, and mental well-being.
Choosing the Right Obstetrician & Gynecologist at drseckin.com
Recognizing the importance of expert care, Dr. Seckin and his team specialize in advanced gynecological surgery, offering state-of-the-art procedures tailored to individual needs. When considering bilateral salpingo-oophorectomy, selecting a skilled obstetrician and gynecologist with extensive experience is paramount for safety, efficacy, and comfort.
The team at drseckin.com is committed to providing comprehensive counseling, personalized care plans, and minimally invasive surgical options to ensure optimal outcomes and a positive patient experience.
Empowering Women Through Knowledge: Making Informed Decisions
Understanding the complexities and benefits of bilateral salpingo-oophorectomy empowers women to make informed healthcare decisions. Whether it is for cancer prevention, symptom management, or treatment of gynecological conditions, being well-informed about surgical options, risks, and long-term health implications is crucial for optimal outcomes.
Consulting with experienced specialists, discussing personal risk factors, and considering genetic testing can guide women toward informed, confident choices regarding their reproductive and overall health.
The Future of Women's Gynecological Surgery
Advances in surgical technology, genetic screening, and personalized medicine continue to transform the landscape of women’s health. Minimally invasive techniques like laparoscopy and robotic surgery have revolutionized recovery times, reduced complications, and improved patient satisfaction.
Furthermore, ongoing research aims to better understand the implications of removing reproductive organs and develop targeted therapies that preserve hormonal function while effectively managing disease.
At the forefront of these innovations, leading clinics such as drseckin.com are dedicated to integrating scientific progress with compassionate, patient-centered care.
Conclusion: Your Health, Your Choice
Bilateral salpingo-oophorectomy is a powerful surgical intervention that plays a vital role in managing ovarian and fallopian tube diseases, including cancer prevention and treatment. With advanced surgical techniques and expert care provided by top obstetricians and gynecologists, women can navigate their health journeys confidently.
Remember, making informed decisions about your gynecological health involves understanding the procedure, its benefits, potential risks, and long-term implications. Partnering with experienced healthcare professionals at drseckin.com ensures that you receive the highest standard of care tailored to your personal needs.
bilateral salpingo-oophorectomy.